7th International RASopathies Symposium: Pathways to Understanding – Expanding Knowledge, Enhancing Research and Therapeutic Discovery
POSTERS
[text in this color range = link to poster]
Posted Alphabetically by Presenting Author’s Last Name
List of Poster Presenters:
- Juan G. Báez Flores
- CFC International – Request for Proposals
- Hilary Berens
- Geoffrey J. Clark
- Allison M. H. Foy
- Green Lab – Research Study
- Lotte E.R. Kleimeier
- Vanesa López González
- Juliana Lores
- Amanda Monty
- Saeideh Nakhaei-Rad
- National Cancer Institute – RASopathies Study
- Noonan Syndrome Association – Start-up Grant
- Rebecca Norcross
- Gerilyn M. Olsen
- Carlos Andrés Quintero Romero and Maria Fernanda Meneses Hernandez
- Katie Ryan
- Samantha Craig Spires
- RASopathies Network – Contact Registry
- RASopathies Network – Future Grant Opportunity
-:- -:- -:-
1. Generation of RASopathies-associated genetic variants for cell-based assays
Juan G. Báez Flores, Mario Rodríguez Martín, Jesús Lacal
Group of Molecular Genetics of Human Diseases. Section of Genetics, Faculty of Biology, University of Salamanca, 37007, Salamanca, Spain.
Salamanca Biomedical Research Institute (IBSAL), 37007, Salamanca, Spain
Contact: alumni.jbaez@usal.es
The RASopathies are developmental syndromes of diverse genetic origin characterized by germline mutations in genes that encode the proteins of the Ras/MAPK pathway. The RASopathies that we study in our lab include neurofibromatosis type 1 (NF1) (MIM ID #162200) and Legius syndrome (LS) (MIM ID #611431), which appear as a result of loss of function mutations in the NF1 and SPRED1 genes, respectively. A total of 6 NF1 variants and 5 SPRED1 variants were generated by PCR site directed mutagenesis into the cloning vectors pBSK and pNZY28, respectively. To facilitate the site-directed mutagenesis workflow with NF1 we have generated two different constructs containing the first and the second half of the NF1 gene. Then, we cloned these variants into the lentiviral expression vector pLVX-IRES-Hyg. These lentiviruses, along with the empty vector and wild-type NF1 and SPRED1 genes were used to generate stable cell lines in order to carry out cell based assays. An in silico approach to predict the potential pathogenicity of the different variants was done using ClinVar, Varsome and Cosmic. Our work will allow us to classify these genetic variants according to their pathogenic potential and to investigate the molecular mechanisms that underlie these mutations.
-:- -:- -:-
2. Family Advocacy Poster: Child with NF1
Hilary Behrens
-:- -:- -:-
3. 2021 Liliian’s Legacy Request for Proposals (RFP)

GRANT OPPORTUNITY Announcement
Amount: up to $30,000 Deadline: September 17, 2021
Potential Focus Areas:
Seizures
Behavior
Sleep disturbances
Presentation in adults
~ Other topics welcome ~
-:- -:- -:-
4. Novel RAS inhibitors for NF1 disease
Howard Donninger1,3; Rachel Ferril2; Destine Ede2; Desmond R. Harrell-Stewart1,2; Joe Burlison1,3; John Trent1,3; and Geoffrey J. Clark1,2
1Molecular Targets Group, James Graham Brown Cancer Center, Departments of 2Pharmacology & Toxicology and 3Medicine, School of Medicine, University of Louisville, Louisville, KY, USA
Neurofibromatosis disease is caused by defects in the NF1 tumor suppressor. NF1 serves as a negative regulator or GAP (GTPase Activating Protein) for the RAS oncoproteins. Consequently, cells with defective NF1 exhibit deregulated RAS oncoprotein activity and this is likely to be a driving event for many of the pathologies of the disease. This includes the development of MPNST (Malignant Peripheral Nerve Sheath Tumors).
We have developed a novel small molecule that directly binds to RAS proteins with low micromolar affinity and inhibits their function by blocking their ability to interact with downstream effector proteins. Here we show that our current lead compound can suppress RAS signaling in MPNST cells and the tumorigenic phenotype of MPNST cell lines in vitro and in vivo. Moreover, we show that we can suppress the growth of primary tumor grafts (pdx) from MPNST patients. The compound exhibits no apparent toxicity in animals and is orally available. Compound optimization is ongoing.
-:- -:- -:-
5. Social Behavior in Children with RASopathies and Idiopathic Autism
Allison M. H. Foy1,2, Rebekah L. Hudock1, Ryan Shanley3, and Elizabeth I. Pierpont1
1Department of Pediatrics, Division of Clinical Behavioral Neuroscience, University of Minnesota Medical School
2Department of Educational Psychology, University of Wisconsin-Madison
3Biostatistics Core, Masonic Cancer Center, University of Minnesota
Contact: Allison Foy – foyxx064@umn.edu
Objective: Children with genetic syndromes that arise from disruptions to the RAS-MAPK cellular signaling pathway (RASopathies) and children with non-syndromic autism spectrum disorder (idiopathic ASD) are both at increased risk of social problems, but few studies have compared social behavior in these conditions. Some literature indicates that children with RASopathies may exhibit relatively strong empathetic or prosocial behaviors. Our study sought to 1) evaluate and compare the presence of empathy and social competence in children and adolescents with RASopathies and idiopathic ASD, and 2) determine which psychological factors predict scores on measures of empathy and social competence for each group.
Participants and Methods: In this cross-sectional, survey-based investigation, parents and caregivers of 180 children with RASopathies (neurofibromatosis type 1, Noonan syndrome, cardiofaciocutaneous syndrome, Costello syndrome) and 97 children with non-syndromic (i.e., idiopathic) ASD provided ratings to evaluate the presence of empathetic behavior and social competence as well as symptoms of hyperactivity/inattention, emotional problems, and communication skills. Medical and family history was also ascertained.
Results: Despite a notably heightened risk for problems with social competence, parent ratings demonstrated relatively intact empathetic behaviors in children with RASopathies. In contrast, among children with idiopathic ASD, parents reported a similar degree of impairment across these two domains of social behavior. Similarities and differences emerged with regard to which psychological factors predicted social behavior in these two groups. Stronger communication skills were associated with increased empathetic behavior for both groups. For the idiopathic ASD group, communication abilities were also associated with social competence. For the RASopathy group, problems with social competence were more strongly associated with emotional challenges and hyperactive-impulsive behaviors.
Conclusions: The development of social behavior among children with RASopathies may involve a distinct pattern of strengths and weaknesses as compared to a behaviorally-defined disorder such as idiopathic ASD. Identification of areas of resilience as well as behavioral and social challenges may support more targeted intervention.
-:- -:- -:-
6. Green Lab’s Research Study
= RESEARCH OPPORTUNITY Announcement =
Focus on the brain and child’s development
-:- -:- -:-
7. Lymphatic anomalies during life in patients with Noonan syndrome and related disorders
Lotte E.R. Kleimeier1, Jessie W. Swarts1, Erika Leenders2, Willemijn M. Klein3, Jos M.T. Draaisma1
1Radboud University Medical Center, Radboud Institute for Health Sciences, Amalia Children’s Hospital, Department of paediatrics, Nijmegen, The Netherlands
2Radboud University Medical Center, Department of Human Genetics, Nijmegen, The Netherlands
3Radboud University Medical Center, Department of Radiology and Nuclear medicine, Nijmegen, The Netherlands
Introduction: Noonan syndrome (NS) has been associated with an increased risk of lymphatic anomalies. An estimated prevalence of 20% has commonly been reported. However, cohort studies are scarce. The prevalence of lymphatic anomalies seem to differ between genetic mutations. Therefore, this study provide an overview of the clinical presentation and prevalence of lymphatic anomalies in patient with NS, NS with multiple lentigines, and NS with Loose anagen hair. In addition, genotype-phenotype correlations will be investigated.
Methods: This retrospective cohort study included patients from the Radboud University Medical Center, who were clinically and genetically diagnosed with NS or related disorders till September 2020.
Results: The study population consisted of 267 patients, with a median age of 18 years (IQR: 9-34). Prenatal lymphatic anomalies most often presented as an increased nuchal translucency and/or chylothorax. Prenatal lymphatic anomalies increased the risk of lymphatic anomalies during infancy (odds ratio 10.5, 95% confidence interval 3.6-30.1). Postnatal lymphatic anomalies most often presented as lymphedema. The lifetime prevalence of lymphatic anomalies was 21%. Genotype-phenotype correlations showed a higher lifetime prevalence in patients with a pathogenic SOS2 or SHOC2 variants compared to NS patients with a pathogenic PTPN11 variant (NS PTPN11 vs SOS2: p=0.01; NS PTPN11 vs SHOC2: p=0.02).
Conclusion: Prenatal and postnatal lymphatic anomalies are common in patients within the NS spectrum. Patients with prenatal lymphatic anomalies had an increased risk of lymphatic anomalies during infancy. An especially high lifetime prevalence of lymphatic anomalies was found in patients with a pathogenic SOS2 or SHOC2 variants.
-:- -:- -:-
8. Clinical and molecular characterization of a group of Spanish and German patients with Noonan syndrome
V. López González1, M. Ballesta-Martínez1, M. Sánchez-Soler1, A. Serrano-Antón1, G. Glover-López2, B. Ezquieta-Zubicaray3, A. Küchler4, B. Albrecht4, D. Wieczorek5, E. Zorio6, C. Lissewski7, M. Zenker7, E. Guillén-Navarro1
1Sección de Genética Médica. Servicio de Pediatría. Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, Spain
2Centro de Bioquímica y Genética Clínica. Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, Spain
3Laboratorio de Diagnóstico Molecular. Hospital General Universitario Gregorio Marañón, Madrid, Spain
4Institut für Humagenetik, Universtitätsklinikum Essen, Essen, Germany
5Institüt für Humangenetik, Universitätsklinikum Düsseldorf, Düsseldorf, Germany
6Servicio de Cardiología. Hospital Universitari i Politècnic La Fe, Valencia, Spain
7Institut für Humangenetik, Universitätsklinikum Magdeburg, Magdeburg, Germany
Contact: vanesa.lopez2@carm.es
Introduction: RASopathies are a group of diseases due to variants in genes that encode components or regulators of the RAS/MAPK pathway. Among them, Noonan syndrome (NS) represents one of the most prevalent disorders of multiple congenital anomalies.
Objective: Clinical and molecular characterization of patients with NS. Estimation of its prevalence, genotype-phenotype correlation analysis, and evaluation of the adequacy of the follow-up to the clinical guidelines.
Material and methods: Retrospective, descriptive and international collaborative study between the Medical Genetics Section, Hospital Clínico Universitario Virgen de la Arrixaca, Murcia, Spain, and the Institut für Humangenetik, Universitätsklinikum, Essen, Germany. Review of medical records of patients with prenatal/postnatal diagnosis of a molecularly confirmed NS diagnosis, between 1994-2012 in Essen and 2002-2018 in Murcia. Collection of clinical, phenotypic data (Face2gene facial recognition program) and genotype.e
Results: 88 cases. Main referral units: General Pediatrics and Pediatric Cardiology. Mean age at referral: 5.79 years. Estimated prevalence for NS: 1/7348 live newborns. Main findings: heart defects (76%), short stature (53%), microcephaly (40%) and intellectual disability (ID) (35%). All those classified as typical met van der Burgt diagnostic criteria compared to 75% of the atypical ones (p=0.003). Statistically significant association between low weight, short stature, microcephaly, motor delay and cardiac surgery with ID, also between central nervous system abnormalities and seizures. PTPN11 was the most frequently mutated gene (74%). Significantly higher percentage of microcephaly in PTPN11 and hypertrophic cardiomyopathy in RAF1. Neurodevelopment and height were less affected in SOS1.
Conclusions: We present a wide series of NS cases with clinical manifestations, mostly, in accordance with previous publications. There is a large prevalence of microcephaly, higher in PTPN11, associated with ID and behavioral abnormalities, not previously reported. There appears to be greater severity of systemic involvement accompanying the severity of the craniofacial phenotype. The lack of complementary examinations constitutes a point of improvement. The estimated prevalence in Murcia is lower than previously reported, the development of strategies to improve its detection being necessary. Greater awareness of adult specialties towards this group of diseases is necessary.
-:- -:- -:-
9. Family Advocacy Poster: Child with CFC/YWHAZ
Amanda Monty
-:- -:- -:-
10. The challenges of RASopathies patients during the COVID-19 pandemic in Colombia (South America)
Juliana Lores1, Eidith Gomez-Pineda2, Carlos E. Prada3, Harry Pachajoa4
1Medical Genetics program, Faculty of Health Sciences, Universidad Icesi, Cali, Colombia. Centro de Investigaciones Clínicas, Fundación Valle del Lili, Cali, Colombia
2Centro de Investigaciones en Anomalías Congénitas y Enfermedades Raras (CIACER), Universidad Icesi, Cali, Colombia
3Division of Human Genetics, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio. Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, Ohio. Fundación Cardiovascular de Colombia, Bucaramanga, Colombia
4Department of Genetics, Fundación Valle del Lili, Cali, Colombia. Centro de Investigaciones en Anomalías Congénitas y Enfermedades Raras (CIACER), Universidad Icesi, Cali, Colombia
Introduction: Since the beginning of the Coronavirus Disease of 2019 (COVID-19) pandemic, countless difficulties have been affecting the daily living of people worldwide. Strict measures of social distancing, personal protective equipment mandates, restricted access to healthcare, impact on economic stability and mental health are all concerns that still affect many people.
People living with rare diseases, like RASopathies, are a particularly vulnerable community greatly impacted by the pandemic. The burden of these challenges can be exacerbated in a country like Colombia with growing economic disparities, an unequitable health system, and delayed access to SARS-CoV-2 vaccination. Our aim was to assess the experiences of RASopathies patients and their families on how the COVID-10 pandemic challenges have impacted their lives, in order to increase public and scientific awareness on the topic.
Methods: Observational cross-sectional study with a convenience sampling strategy between April 1st and May 15th, 2021. A questionnaire adapted from previous published research on COVID-19 pandemic and quality of life or related publications was designed. It was addressed to patients/caregivers living with a RASopathy, who were contacted via phone call. Twenty replies were obtained. None of the replies were excluded. Descriptive statistical analysis was performed. Absolute frequencies and percentages were used.
Results: A total of 20 individuals (19 caregivers and 1 patient) were included in this study. All of them live in the south-west region of Colombia, with the exception of two individuals from the Amazonas department (far south of Colombia). The majority of patients (14/20, 70%) have a diagnosis of Noonan syndrome (NS), followed by neurofibromatosis type 1 (4/20, 20%), NS with multiple lentigines (1/20, 5%) and NS with loose anagen hair (1/20, 5%).
Household composition was primarily of three or four individuals, with one patient diagnosed with a RASopathy (17/20, 85%). Employment was distributed as: employed (11/20, 55%), stay-at-home parent (5/20, 25%), unemployed and fit to work (3/20, 15%), and other status (2/20, 10%). Restricted access to testing and follow-up by specialist was reported by the majority of individuals (15/20, 75%). Difficulty to schedule an appointment with a geneticist was widely reported (11/20, 55%), and access to telemedicine greatly varied between specialties, with most patients having a positive experience (7/9, 77.7%). Trouble with access to medication for those with pharmacologic treatment was stated (5/16, 31.2%), and with access to therapies (12/16, 75%). Delay in surgical management was common (7/10, 70%).
Most caregivers reported leaving their home only for essential activities (12/20, 60%), while the rest stated to leave the house daily for work. Almost all caregivers described the level of health threat as very high or high for the patients and reported full adherence to mask mandate (18/20, 90%). Generally, families felt that economic difficulties, social isolation, and restricted healthcare access were the main challenges for patients during the pandemic (19/20, 95%). 5 caregivers have been able to receive a vaccine against SARS-CoV-2 (26.3%). Only 2 individuals reported hesitancy to vaccination.
Conclusions: RASopathies patients and caregivers have been greatly affected by the economic difficulties, social isolation, and restricted healthcare access that the COVID-19 pandemic has caused. Health disparities and limited access to vaccination can delay solutions to these challenges. Important measures need to be implemented in order to address these limitations and provide patients with the multidisciplinary care they need.
-:- -:- -:-
11. Alteration of myocardial structure and function in RAF1-associated Noonan syndrome
Saeideh Nakhaei-Rad1, Farhad Bazgir2, Marcel Bucholzer3, Fereshteh Haghighi4, Julia Dahlmann5, Anne Schänzer6, Andreas Hahn7, Sebastian Kötter8, Denny Schanze9, Ruchika Anand10, Florian Funk11, Andrea Borchardt12, Annette Vera Kronenbitter13, Jürgen Scheller14, Roland P. Piekorz15, Andreas S. Reichert16, Marianne Volleth17, Matthew J. Wolf18, Lukas Cyganek19, Bruce D. Gelb20, Marco Tartaglia21, Joachim Schmitt22, Martina Krüger23, Martin Zenker24, George Kensah25, Mohammad R. Ahmadian26
1Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; Stem Cell Biology and Regenerative Medicine Research Group, Institute of Biotechnology, Ferdowsi University of Mashhad, Mashhad, Iran; s.nakhaeirad@um.ac.ir
2Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; farhad.bazgir@hhu.de
3Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; buchholzer.marcel@gmail.com
4Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; Department of Thoracic and Cardiovascular Surgery, University Medical Center, Göttingen, Germany; fereshteh.haghighi@med.uni-goettingen.de
5Department of Thoracic and Cardiovascular Surgery, University Medical Center, Göttingen, Germany; dahlmann.julia@mh-hannover.de
6Institute of Neuropathology, Justus Liebig University Giessen, Giessen, Germany; Anne.Schaenzer@patho.med.uni-giessen.de
7Department of Child Neurology, Justus Liebig University Giessen, 35392 Giessen, Germany; Andreas.Hahn@paediat.med.uni-giessen.de
8Institute of Cardiovascular Physiology, Duesseldorf, Germany; sebastian.koetter@uni-duesseldorf.de
9Institute of Human Genetics, University Hospital, Otto von Guericke-University, Magdeburg, Germany; denny.schanze@med.ovgu.de
10Institute of Biochemistry and Molecular Biology I, Medical Faculty and University Hospital Düsseldorf, Heinrich-Heine-University Düsseldorf, Düsseldorf, Germany; Ruchika.Anand@uni-duesseldorf.de
11Institute of Pharmacology and Clinical Pharmacology, Duesseldorf University Hospital, Duesseldorf, Germany; florian.funk@hhu.de
12Institute of Biochemistry and Molecular Biology I, Medical Faculty and University Hospital Düsseldorf, Heinrich-Heine-University Düsseldorf, Düsseldorf, Germany; Andrea.Borchardt@uni-duesseldorf.de
13Institute of Pharmacology and Clinical Pharmacology, Duesseldorf University Hospital, Duesseldorf, Germany; Annette.Kronenbitter@uni-duesseldorf.de
14Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; jscheller@hhu.de
15Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; Roland.Piekorz@uni-duesseldorf.de
16Institute of Biochemistry and Molecular Biology I, Medical Faculty and University Hospital Düsseldorf, Heinrich-Heine-University Düsseldorf, Düsseldorf, Germany; reichert@hhu.de
17Institute of Human Genetics, University Hospital, Otto von Guericke-University, Magdeburg, Germany.
18Department of Medicine and Robert M. Berne Cardiovascular Research Center, University of Virginia, USA; MJW5MC@hscmail.mcc.virginia.edu
19Stem Cell Unit, University Medical Center Göttingen, 37075 Göttingen, Germany;
20Mindich Child Health and Development Institute and Departments of Pediatrics and Genetics and Genomic Sciences, Icahn School of Medicine at Mount Sinai, New York, NY 10029, USA; bruce.gelb@mssm.edu
21Genetics and Rare Diseases Research Division, Ospedale Pediatrico Bambino Gesù, IRCCS, 00146 Rome, Italy; marco.tartaglia@opbg.net
22Institute of Pharmacology and Clinical Pharmacology, Duesseldorf University Hospital, Duesseldorf, Germany; joachim.schmitt@uni-duesseldorf.de
23Institute of Cardiovascular Physiology, Duesseldorf, Germany; martina.krueger@uni-duesseldorf.de
24Institute of Human Genetics, University Hospital, Otto von Guericke-University, Magdeburg, Germany; martin.zenker@med.ovgu.de
25Department of Thoracic and Cardiovascular Surgery, University Medical Center, Göttingen, Germany; george.kensah@med.ovgu.de
26Institute of Biochemistry and Molecular Biology II, Medical Faculty of the Heinrich Heine University, Duesseldorf, Germany; reza.ahmadian@uni-duesseldorf.de
RASopathies, including Noonan syndrome (NS), are caused by germline variants in genes encoding components of the RASMAPK pathway. Distinct variants, such as the recurrent Ser257Leu substitution in RAF1, are associated with severe hypertrophic cardiomyopathy (HCM). Here, we explored as part of the NS phenotype the elusive mechanistic link of NSassociated RAF1S257L to HCM using three-dimensional cardiac bodies and bioartificial cardiac tissue, differentiated from -patient-derived (RAF1, Ser257Leu) induced pluripotent stem cells (iPSCs). The results revealed molecular, cellular, structural and functional impacts on the myocardium, and elucidated the link of RAF1S257L hyperactivity to hypertrophic myocardial remodeling. Strikingly, electron micrographs of the Zline area revealed the shortening of I-bands in both iPSC-derived RAF1S257L cardiomyocytes and a cardiac biopsy of a NS patient, linked to which may be caused by aberrant phosphorylation of the giant intra-sarcomeric protein Titin. Remarkably, this phenotype was reverted by using the MEK inhibitor PD0325901. Collectively, our findings uncovered a direct link between a RASopathy gene variant and abnormal sarcomeric structure and cardiac function forming the basis for future therapeutic approaches.
-:- -:- -:-
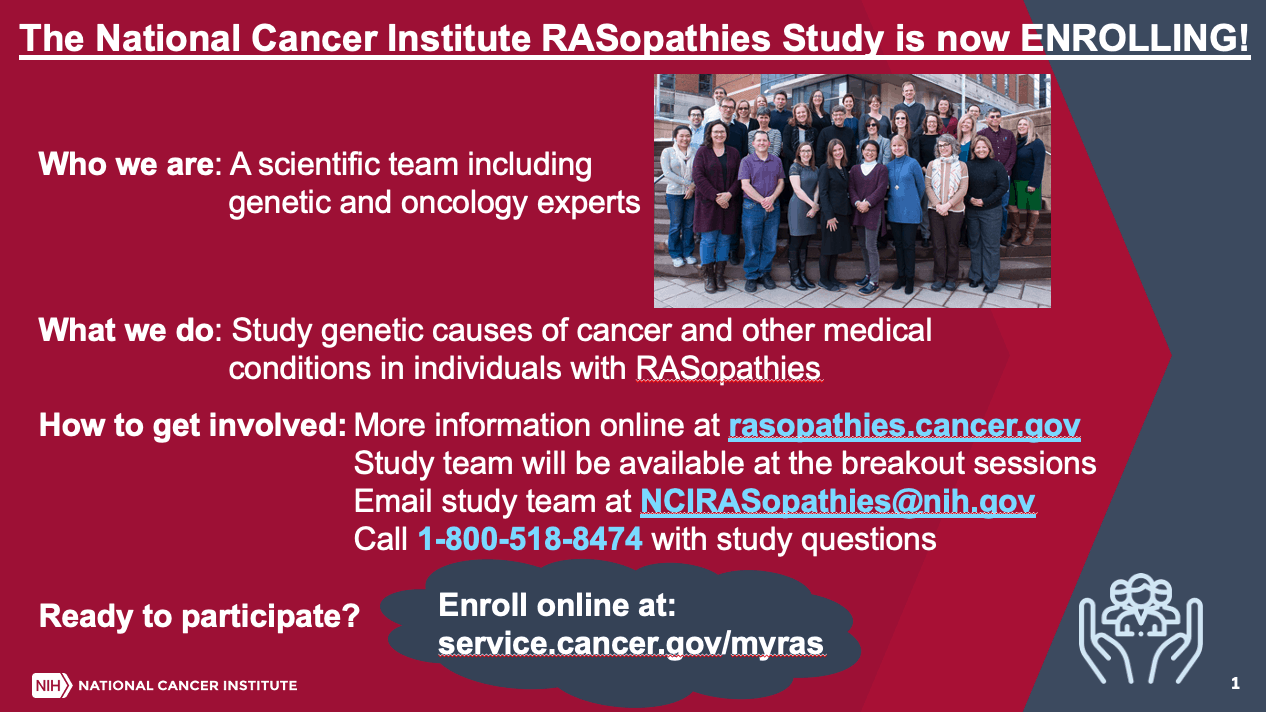
12. NCI RASopathies Study
-:- -:- -:-
13. Start Up Grant

= GRANT OPPORTUNITY Announcement =
The Trustees of the UK Noonan Syndrome Association (NSA) are pleased to invite applications for start-up research funding into Noonan Syndrome from the International RASopathy research community.
Applications for the current “Start Up Grant” of £20,000 (US$27,500) are welcome on any date before the closing date on 29th October 2021. No applications will be considered after that date.
In 2014 the charity advertised and then awarded a similar start up grant to Professor Sahar Mansour and the Lymphoedema Research Group at St Georges in London to investigate the lymphatic abnormalities in Noonan syndrome. They were able to identify a new genetic cause of lymphoedema and develop radiological techniques for imaging the lymphatic vessels. On the back of this start up grant together with the results generated from the research they were able to secure around £2million further research funding.
The charity wishes to make a further “Start Up grant” of £20,000 (US$ 27,500). This grant is for researchers to undertake innovative research in relation to Noonan Syndrome or related syndromes. This may be for a complete project but is more likely to provide the preliminary data to allow the research group to be successful in obtaining a larger project grant to support further research into Noonan syndrome. The grant is designed to develop a new area of research rather than complete an existing project.
The trustees have identified a number of areas of interest and concern to families. These are:
- Further understanding of the RASopathy pathway for development of new treatments
- Understanding the basis of joint and muscle pain
- Development of the brain with particular reference to epilepsy
- Improved management of heart abnormalities
- Speech and feeding difficulties in infancy
Applications are not limited to these areas, although they do reflect current family concerns for further help.
For further information from Professor Michael Patton (Medical Advisor) or Sandie Dent (Charity Manager) together with application forms, contact: research@noonansyndrome.org.uk
-:- -:- -:-
14. Shoc2 is a pivotal regulator of neural crest specification, migration, and differentiation
Rebecca Norcross, Lina Abdelmoti, Daileen Landestroy, Olivia Tussey, and Emilia Galperin
Dept. of Molecular and Cellular Biochemistry, University of KY, Lexington, KY 40536, USA
Contact: Emilia Galperin – emilia.galperin@uky.edu
RASopathies collectively account for one of the most common genetic disorders with phenotypic severity ranging from mild to fatal. Patients with RASopathies exhibit diverse developmental defects including cartilage and bone dimorphisms, cardiac abnormalities, growth delays, irregular skin pigmentation, and defective enteric nervous systems. Most affected tissues arise from a transient, stem cell-like progenitor cell population, neural crest (NC). Thus, uncovering the underlying pathogenicity mechanisms governing NC cells during embryogenesis can potentially lead to the development of RASopathy treatments.
In this study, we focus on elucidating the molecular mechanism by which Shoc2-mediated signals through the Ras-Raf pathway regulate the development of NC. Shoc2 is a non-enzymatic scaffold protein that is essential for embryonic development. It is the only scaffold protein in which gene mutations have been identified in RASopathy (Noonan syndrome with loose anagen hair) patients. However, the molecular details delineating Shoc2-mediated signals in NC are undetermined. Therefore, we investigated how the loss of Shoc2 affects the expression of NC regulatory network genes and different stages of NC development. In our experiments we depleted Shoc2 using a morpholino and analyzed gene expression by whole in situ hybridization and RT-qPCR analysis.
We found that the expression of early neural plate border formation regulators, prdm1a, pax7, and foxD3 were affected by the loss of Shoc2. Embryos depleted of Shoc2 also had irregular spatial organization and expression of NC markers foxD3 and sox10 and the cell migratory gene dlx2a during the subsequent NC cell specification and migration processes. Additionally, during terminal cell differentiation into mature NC-derived Schwann cells, the expression of krox20 (required for myelin production) was deficient. This suggests that NC cells are unable to overcome the early NC defects from deficient Shoc2 signaling. Finally, we determined that Shoc2-mediated signaling is essential for the regulation of cartilage proteoglycan genes’ (acana and acanb) expression. Ultimately, depleting Shoc2 leads to abnormal NC development and deficient downstream NC-derived cell tissues.
Thus, we conclude that Shoc2 is required for the neural plate border formation during gastrulation. Furthermore, Shoc2 is essential for NC cell specification, migration, and terminal differentiation. Finally, the changes of acana and acanb expression indicate that Shoc2- transmitted signals are essential for the regulation of the tightly controlled structural proteins required for craniofacial anatomy. For the first time, this study has defined the foundational mechanism of Shoc2-deficient RASopathy phenotypes in zebrafish embryos that recapitulate patient Noonan syndrome with loose anagen hair. In conclusion, Shoc2 is critical for NC development from initial induction to final cell migration and differentiation. Ultimately, the abnormalities caused from irregular Shoc2-mediated signaling have long-lasting anatomical defects founded by irregularly expressed extracellular matrix proteins.
-:- -:- -:-
15. Pathogenesis and treatment of papillomas in Costello Syndrome
Gerilyn M. Olsen, MD1, Pau Castel, PhD2, Luke Johnson, MD3, Alfons Krol, MD4, Sabra Leitenberger, MD4, Kevin White, MD4, Dawn Siegel, MD1
1Medical College of Wisconsin
2University of California, San Francisco
3University of Utah
4Oregon Health & Science University
Contact: Gerilyn Olsen – golsen@mcw.edu
Costello syndrome (CS) is caused by a mutation in the regulatory HRAS gene, leading to constitutive activation of the RAS/Mitogen-Activated Protein Kinase (MAPK) pathway. Dysregulation of RAS/MAPK has long been implicated in cancer pathogenesis, but more recently it has been identified as the cause of several developmental syndromes, including CS. Individuals with Costello syndrome have distinctive dermatologic findings, such as cutaneous papillomas, particularly around the nares and alar rim, palmoplantar keratoderma, acanthosis nigricans, and generalized hyperpigmentation. In some patients, the papilloma burden can be quite high, and patients may find the numerous lesions to be irritating or stigmatizing. The papillomas are often refractory to topical treatments and may require removal with snip excision, cryotherapy, or cautery. It remains unknown whether these lesions are due to human papillomavirus (HPV) infection or constitutive activation of the MAPK pathway in keratinocytes.
Here, we report 10 patients with CS confirmed by genetic analysis who desired removal of papillomas. Four of the tissue samples were tested for HPV at the time of removal, all of which were negative; this finding supports the theory that papillomas in CS may be caused by mosaic second hit mutations, rather than viral infection. Whole exome sequencing is planned for 4 patients who have papilloma samples available for comparison. A better understanding of the pathogenesis of Costello associated papillomas will lead to targeted and improved treatment options for patients.
References
1. Siegel DH, Mann JA, Krol AL, Rauen KA. Dermatological phenotype in Costello syndrome: consequences of Ras dysregulation in development: Dermatological phenotype and Ras dysregulation in Costello syndrome. British Journal of Dermatology 2012; 166:601–7
2. Gripp KW, Morse LA, Axelrad M, et al. Costello syndrome: Clinical phenotype, genotype, and management guidelines. Am J Med Genet 2019; 179:1725–44.
3. Chen X, Mitsutake N, LaPerle K, et al. Endogenous expression of HrasG12V induces developmental defects and neoplasms with copy number imbalances of the oncogene. PNAS 2009; 106:7979–84.
-:- -:- -:-
16. Family Advocacy Poster: Adult with NS/BRAF
Katie Ryan
-:- -:- -:-
17. Proposal of an algorithm for the syndromic and molecular diagnosis of RASopathies based on HPO nomenclature
Carlos Andrés Quintero Romero1 and Maria Fernanda Meneses Hernandez1, Diana Ramirez-Montaño2, Harry Pachajoa3, Juliana Lores4
1Faculty of Health Sciences, Universidad Icesi, Cali, Colombia
2Center for Research in Congenital Anomalies and Rare Diseases (CIACER), Faculty of Health Sciences, Universidad Icesi, Cali, Colombia
3Department of Genetics, Fundación Valle del Lili, Center for Research in Congenital Anomalies and Rare Diseases (CIACER), Universidad Icesi, Cali, Colombia
4Medical Genetics Program, Faculty of Health Sciences, Universidad Icesi, Cali, Colombia
Introduction: RASopathies are a heterogeneous set of genetic syndromes caused by germline mutations in genes encoding components or regulators of the RAS/mitogen-activated protein kinase (MAPK) pathway; each RASopathy expresses a characteristic phenotypic pattern; however, common mechanisms of Ras/MAPK pathway dysregulation result in overlapping clinical manifestations. Currently, only clinical criteria are available for the diagnostic approach of Neurofibromatosis 1 and Noonan syndrome; while other rasopathies lack a clinical standard for their diagnosis, in addition to this exists limited skill in identifying typical phenotypes by health personnel, which hinders the timely diagnosis of these syndromes; due to this, we proposed the elaboration of an algorithm for the syndromic and molecular diagnostic approach in patients with suspected RASopathies based on the clinical phenotypic characteristics found in the literature with the Human Phenotype Ontology HPO tool.
Methods: A search was performed in the literature and in the HPO library of the phenotypic findings for each of the RASopathies. It was determined that the algorithm should include short stature as a common characteristic due to its high frequency among the syndromes that present the greatest challenge in clinical diagnosis, In addition, the phenotypic findings were classified according to a systemic approach that included elements of dermatology, cardiology, urology, among others, with which high frequency phenotypic patterns were designed for each of the main syndromes within the RASopathies and in selected cases high frequency phenotypic patterns were designed for mutations in specific genes within the syndromes; These phenotypic patterns were integrated into a diagnostic algorithm that is capable of suggesting a clinical and molecular diagnostic impression for the patients. This is linked to a population-based registry database of patients with clinically suspected and confirmed molecular diagnosis of RASopathies; this project is currently under development; it is planned to validate the functionality and diagnostic capability of the algorithm in the patients of the aforementioned registry.
Expected results: It is expected that by submitting the algorithm to the validity test using the patients present in the database, data will be obtained that will allow us to know the intrinsic and extrinsic characteristics of the diagnostic algorithm (sensitivity, specificity, positive predictive value, negative predictive value, etc).
Conclusions: At the moment no similar research has been published that seeks to establish a methodical and standardized approach for the clinical and molecular diagnosis of RASopathies based on clinical findings, it is expected that the results obtained will allow us to reach the conclusion to recommend/reject the clinical and molecular diagnostic algorithm presented.
The limitations of this research include the limited number of patients for certain syndromes (cardio-facial-cutaneous syndrome, Legius syndrome and Costello syndrome) and the absence of a detailed analysis of the publication bias present in the study.
:- -:- -:-
18. Family Advocacy Poster: Child with NS/RIT1
Samantha Craig Spires
-:- -:- -:-
19. RASopathies Network Contact Registry
The RASopathies Contact Registry is a way for families to learn more about research studies they may want to participate in.
- We keep your information confidential
- We do not share it outside the RASopathies Network
We use the information collected to determine whether you might be a good fit for a research study we learn about, so that if you are, we can contact you to decide if you want to reach out to the researcher.
Contact: lschill@rasopathiesnet.org
-:- -:- -:-
20. RASopathies Network MDBR Grant Opportunity